Epilepsy Surgery Update
Epilepsy surgery is one of the main areas of functional neurosurgery. It concerns patients with severe epilepsy, due to the frequency of their seizures or the symptoms they present during them, whose seizures are resistant to antiepileptic drugs (known as pharmaco-resistant epilepsy), and in whom a clinical and paraclinical assessment will demonstrate a focal origin of the seizures (i.e. originating from a lesion or a precise and limited region of the brain).
- Dr Francine Chassoux, Neurologist
- Pr Bertrand Devaux, Neurosurgeon
- Pr Emmanuel Mandonnet, Neurosurgeon
- Dr Adrien Zanin, Neurology, Head of Clinic
- Ms Agathe Laurent, Neuropsychologist
- Ms Aicha Idali, Nurse Coordinator, EEG Technician
It was in Montreal, Canada, in the late 1920s, under the impetus of Wilder Penfield, that this surgery first saw the light of day. In France, it was developed at the Hôpital Sainte-Anne in Paris, thanks to the innovative spirit of neurosurgeon Jean Talairach and neurologist Jean Bancaud, in the late 1950s. Over the years, their students have imported this surgery to their respective centers in France and abroad. There are now around twenty centers in France.
Epilepsy affects 0.5 to 1% of the population. Not only does it lead to disability due to repeated seizures, it also has cognitive, side-effects of anti-epileptic drugs, and psycho-social consequences. It leads to excess mortality, from accidents or SUDEP (sudden unexplained death in epileptic patients). It is estimated that between 5,000 and 10,000 people are potential candidates for a procedure, whereas 400 to 500 procedures are carried out annually in French centers. Delays in treating candidates for surgery are still excessive, especially in children and adolescents, where epilepsy is most likely to begin.
Patients eligible for epilepsy surgery
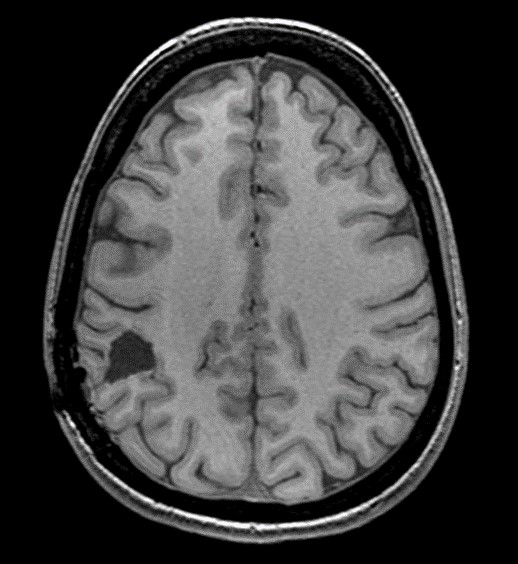
The main surgically curable syndromes are mesiotemporal epilepsy (associated with hippocampal sclerosis) (Figure 1), epilepsy caused by a congenital tumour (known as neurodevelopmental epilepsy) or by a malformation of the cerebral cortex (the most common is focal cortical dysplasia). More rarely involved are vascular malformations (cavernomas) and scarring lesions.

Brain MRI: image of hippocampal sclerosis: atrophy of the left hippocampus (arrow)
Pre-surgical check-up
Potential candidates are selected on the basis of clinical data, EEGs and brain imaging from epilepsy patients undergoing neurological or neuropediatric consultations. Long-term video-EEG recording is usually performed to confirm the focal origin of seizures and correlate it with clinical and imaging data. This initial assessment may be sufficient to establish a surgical indication. It is then complemented by a pre-surgical workup that includes a more specific MRI, with a functional study, coupled with a PET (positron emission tomography) scan, and a neuropsychological workup. In some patients, intracerebral exploration using deep implanted electrodes (SEEG – stereo-electro-encephalography) (figure 2) may be necessary to identify the epileptogenic zone and define the surgical strategy.
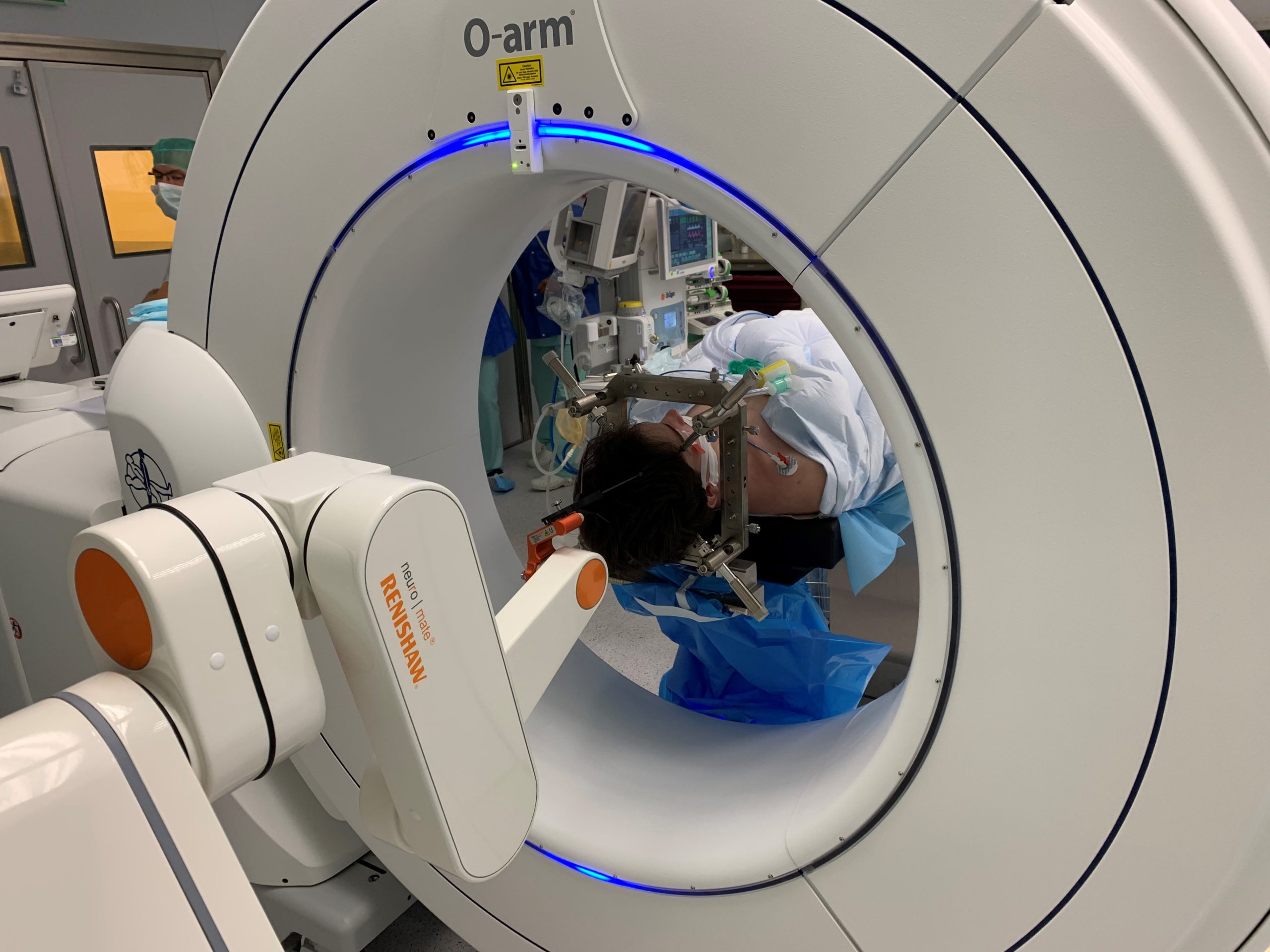
Implantation of electrodes for SEEG exploration

Implantation of electrodes for SEEG exploration
Surgical techniques
Surgical techniques have diversified over the last 4 decades, and today combine resection proceduresThese are the most commonly used and adapted to each patient (Figure 3), those of focal destruction (radiosurgery, stereotactic thermocoagulation), those of disconnection (hemispheric or lobar) and those of neuromodulation (deep brain stimulation and vagus nerve stimulation). Functional brain regions are no longer inaccessible to a surgical procedure that is effective on seizures and respects functional structures. Highly epileptogenic lesions, such as focal cortical dysplasia, can be completely resected without unacceptable functional risk and with excellent seizure results.

Surgical resection of right parietal focal cortical dysplasia.
Surgery results
The results of surgery on seizures depend on the etiology of the epilepsy and the quality of the surgical resection. In mesiotemporal epilepsy, 60-80% of patients who undergo surgery can expect to be seizure-free; over 80% after resection of a neurodevelopmental tumor (DNT, ganglioglioma), and almost 90% after resection of focal cortical dysplasia. Long-term seizure suppression is associated with improved quality of life, reduced mortality and fewer side-effects from chronic epilepsy, and drug treatments can be reduced or even stopped in the best cases, not to mention a reduction in the cost of the disease.
Post-operative MRI showing the resection cavity, sufficient for seizure healing.
Outlook
There is still progress to be made in this functional surgery.
The first are organizational, aimed at earlier identification of good candidates for surgery in the epilepsy patient population, and reducing delays in access to pre-surgical assessment and surgery, by creating care networks, particularly during the child-adult transition; they also concern post-operative follow-up, which determines the quality of surgical results.
The second is technological, with advances in preoperative imaging (ultra-high-field MRI), making it possible to identify brain lesions that are invisible on routine imagers; with improvements in surgical techniques (development of less invasive focal techniques that are still effective); with the development of high-resolution surgical imaging methods (fluorescence imaging, OCT, ultrasound), for more precise real-time guidance of the surgical procedure.)
A multidisciplinary activity
Epilepsy surgery is a multi-disciplinary activity, requiring expertise in various fields – neurology, neurosurgery, neurophysiology, neuroanesthesia, neuroimaging, neuropathology – an experienced paramedical and medico-social team – neuropsychologists, EEG technicians, IDEs, social workers – as well as specific architectural and technical equipment – recording rooms and monitoring stations, implantable medical devices -. It is performed in hospitals that have all the skills and equipment on site.
Projet Epiliepsie – Nouveau Lariboisière
With the support of the University of Paris and GHU-Nord, the new Lariboisière hospital project includes epilepsy surgery. It has the environment needed to develop this functional neurosurgery activity, and is committed to recruiting the human skills, training staff and acquiring the equipment essential to the practice of this surgery in all its aspects: quality care, teaching and training, research.
