The spinal column is made up of vertebrae and intervertebral discs.
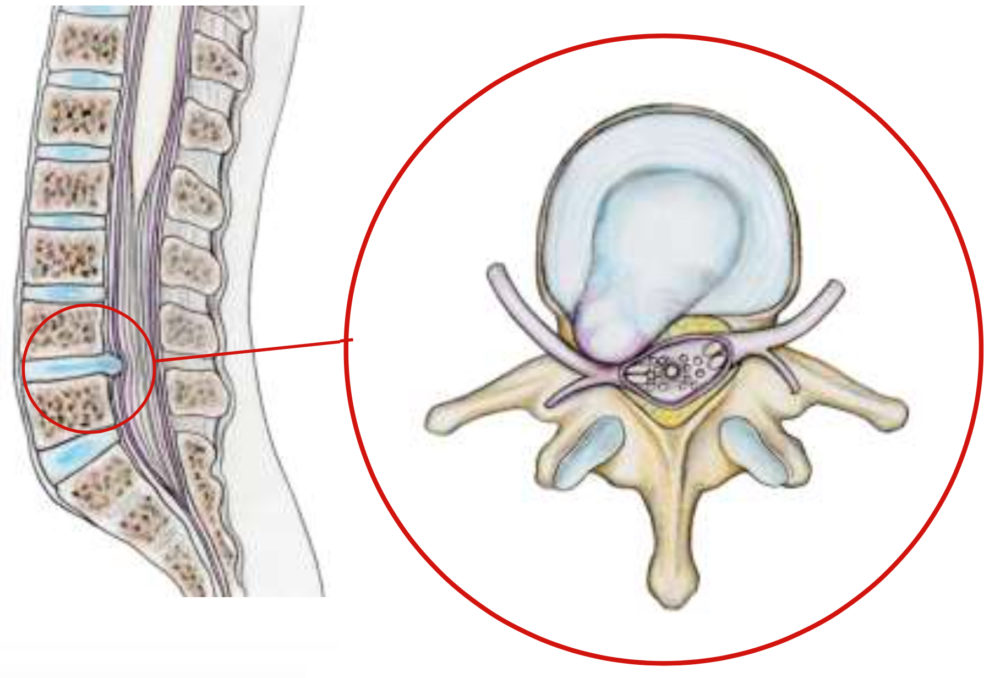
Intervertebral discs are cushions placed between each vertebra, allowing movement by absorbing shocks. They are made up of a fibrous peripheral ring called the annulus and a more gelatinous central part, the nucleus, capable of deforming and resisting compression. This separation between the peripheral and central parts diminishes with age. Under the effect of age, smoking, repeated trauma and genetic factors, the disc becomes fragile and dehydrated. Sometimes, part of the disc migrates through the annulus into the spinal canal, where the dural sac and nerves are located, and compresses one of them. This is known as a herniated disc.
It most often occurs in the lower back, and can lead to compression and inflammation of the lumbar spinal nerves. Pain in the buttock, thigh, leg and foot (sciatica) may be experienced, as well as loss of feeling and weakness, sometimes leading to paralysis.
Surgical treatment is carried out in very specific cases, following a complete assessment and the failure of conservative treatments (medication, physiotherapy, etc.). In the event of extremely intense pain resistant to all analgesics, paralysis or sphincter disorders, emergency surgery may be required. If such symptoms occur, you should seek urgent medical attention.

The symptoms of a herniated disc vary considerably depending on the location of the herniation and your own reaction to the pain. If you have a herniated lumbar disc, you may feel pain radiating from your lower back, down one or both legs and sometimes to your feet (called sciatica). You may feel pain similar to an electric shock.
Activities such as bending, lifting, twisting and sitting can trigger or increase pain. Lying flat on your back with knees bent, or on your side in a “dog-leg” position, can provide relief, as it reduces the pressure exerted on the disc.
Sometimes the pain is accompanied bynumbness and tingling in the leg or foot. It can also be associated with cramps or muscle spasms in the back or leg.
In addition to pain, you may experience muscle weakness in the leg, with a reduction or loss of reflexes in the knee or Achilles tendon. In the case of paralysis, the foot may fall when walking and the toe rubs on the ground. The knee may give way when walking and the leg may give way, leading to a fall. This means that the muscles of the thigh or leg are paralyzed. Likewise, the bladder can become paralyzed, with urine retention followed by urine loss. These are signs of seriousness. If you experience leg weakness or bladder control difficulties, you should seek immediate advice from a neurosurgical department.
The hernia may migrate backwards during a false movement : lifting effort, moving house, violent sporting gestures….. It can also occur spontaneously without any triggering factor. Aging plays an important role. With age, discs dry out and become progressively softer and more pasty. The fibrous outer wall of the disc may weaken, allowing the herniation to migrate. Migration of the herniated disc through the posterior part of the annulus is the cause of back pain, which can be extreme: lumbago with a sensation of “blockage”. Compression of the nerve by the hernia causes pain in the leg.
Genetics, smoking and a number of occupational and recreational activities can lead to early degeneration of the disc.
Herniated discs are more common in people aged between 30 and 40, although middle-aged and older people are at slightly greater risk if they engage in strenuous physical activity.
Lumbar disc herniation is one of the most common causes of lower back pain associated with leg pain. Disc herniations occur less frequently in the cervical region (neck) and much more rarely in the thoracic region in the middle of the back, as this segment of the spine is not very mobile.
How is a diagnosis made?
When you feel pain, consult your family doctor. Your doctor will review your medical history and interview you to understand your symptoms. Next, a clinical examination will be carried out to clarify the pain and look for any muscle weakness or numbness.
Your doctor may prescribe one or more tests: X-ray, MRI, CT scan or EMG.
MRI
: MRI is the examination of choice, as it is much more precise than a CT scan. An MRI can detect which disc is damaged and whether there is nerve compression. It can also detect a bone outgrowth, or another diagnosis such as a narrow lumbar canal, a slippage of one vertebra on another (spondylolisthesis), a tumor ….- CT scan: CT scans can also be useful in treatment strategy, as they provide excellent visualization of vertebral bone, complementing MRI, which provides excellent visualization of soft tissues, discs and nerves.
Electromyogram
is used to determine which nerve is affected by the hernia, in case of doubt on clinical examination and imaging. It measures conduction velocity in the nerves. Small needles are placed in your muscles and the results are recorded on a special machine.
What treatments are available?
Conservative non-surgical treatment is the first step and may include medication, rest, physiotherapy, home exercise, epidural steroid injections, gentle manipulation by an osteopath and pain management. With a well-managed medical approach, 80% of people suffering from back pain or sciatica see their pain diminish or disappear after around 6 weeks, and return to normal activity. If you do not respond to conservative treatment, your doctor may refer you to a neurosurgeon to discuss the possibility of surgery.
-
Non-surgical treatments
Personal care:
In most cases, the pain caused by a herniated disc will subside in a few days and disappear completely in 4 to 6 weeks simply by reducing activity a little.
Medications:
your doctor may prescribe analgesics, non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants and/or corticosteroids.
Non-steroidal anti-inflammatory drugs are used to reduce inflammation and relieve pain.
Analgesics can relieve pain, but do not have the anti-inflammatory effects of NSAIDs. Long-term use of analgesics and NSAIDs can cause stomach ulcers, as well as kidney and liver problems.
Muscle relaxants may be prescribed to control muscle spasms.
Corticosteroids may be prescribed to reduce nerve inflammation. They are taken orally in reduced doses over a short period of a few days. They have the advantage of providing faster pain relief within 24 hours, but can have significant side effects with prolonged use.
Corticosteroid injections:
the procedure is performed under X-ray and consists of an injection of corticosteroids and an anesthetic agent into the epidural space of the spine. The drug is administered close to the painful area to reduce inflammation of the nerves locally. Around 50% of patients will notice relief after an epidural injection, although results tend to be temporary. Repeated injections may be required to achieve the full effect. The duration of pain relief varies, from weeks to years.
Physiotherapy:
the aim is to help you return to full activity as soon as possible and prevent recurrence. Physiotherapists can explain proper posture, lifting and walking techniques. They will work with you to strengthen your lower back, legs and abdominal muscles. They will also encourage you to stretch and increase the flexibility of your spine and legs. Muscle-strengthening exercises are a key part of your treatment and should be continued throughout life.
Holistic therapies:
Some patients find acupuncture, meditation and biofeedback helpful in managing pain and improving their overall health.
-
Surgical treatment:
Surgery for a herniated lumbar disc may be an option if your symptoms do not improve significantly with conservative treatments, or if the pain becomes intolerable and is not relieved by strong painkillers. Surgery may also be recommended if you show signs of nerve damage, such as weakness or loss of sensation in your legs.
Microsurgical discectomy:
the surgeon makes a small incision in the middle of the back. To reach the damaged disc, the muscles of the spine are pulled apart to expose the vertebra. The space between the two vertebrae is opened by removing the ligament that runs from one to the other (yellow ligament), and part of the bone is removed to expose the nerve root and disc. The piece of disc compressing the nerve is carefully removed using special instruments and under a microscope. Around 90% of patients recover quickly and well from this surgery, and can return to their normal work after around six weeks.
Minimally invasive microendoscopic discectomy: the surgeon makes a small incision in the back. Small tubes, called dilators, are used with increasing diameter to widen a tunnel to the vertebra. A small section of bone is removed to expose the nerve root and disc. The surgeon uses an endoscope or microscope to remove the piece of disc that is compressing the nerve root. This technique causes less muscular injury than a traditional discectomy, and enables faster recovery. It is not applicable to all herniated discs.
Post-operative period: relief is usually immediate. The prescribed convalescence period after surgery is approximately 4 to 6 weeks, with a follow-up consultation at the end of this period. During this period, the patient gradually resumes his or her activities, without straining, and avoiding risky movements. Painkillers are generally prescribed for post-operative back pain around the operated area. They are usually very limited. Physiotherapy is also often suggested. Convalescence in a specialized center is rarely necessary. Sporting activities are generally resumed gradually after the recovery period. Depending on the patient’s professional activity, it may be necessary to return to work part-time.
