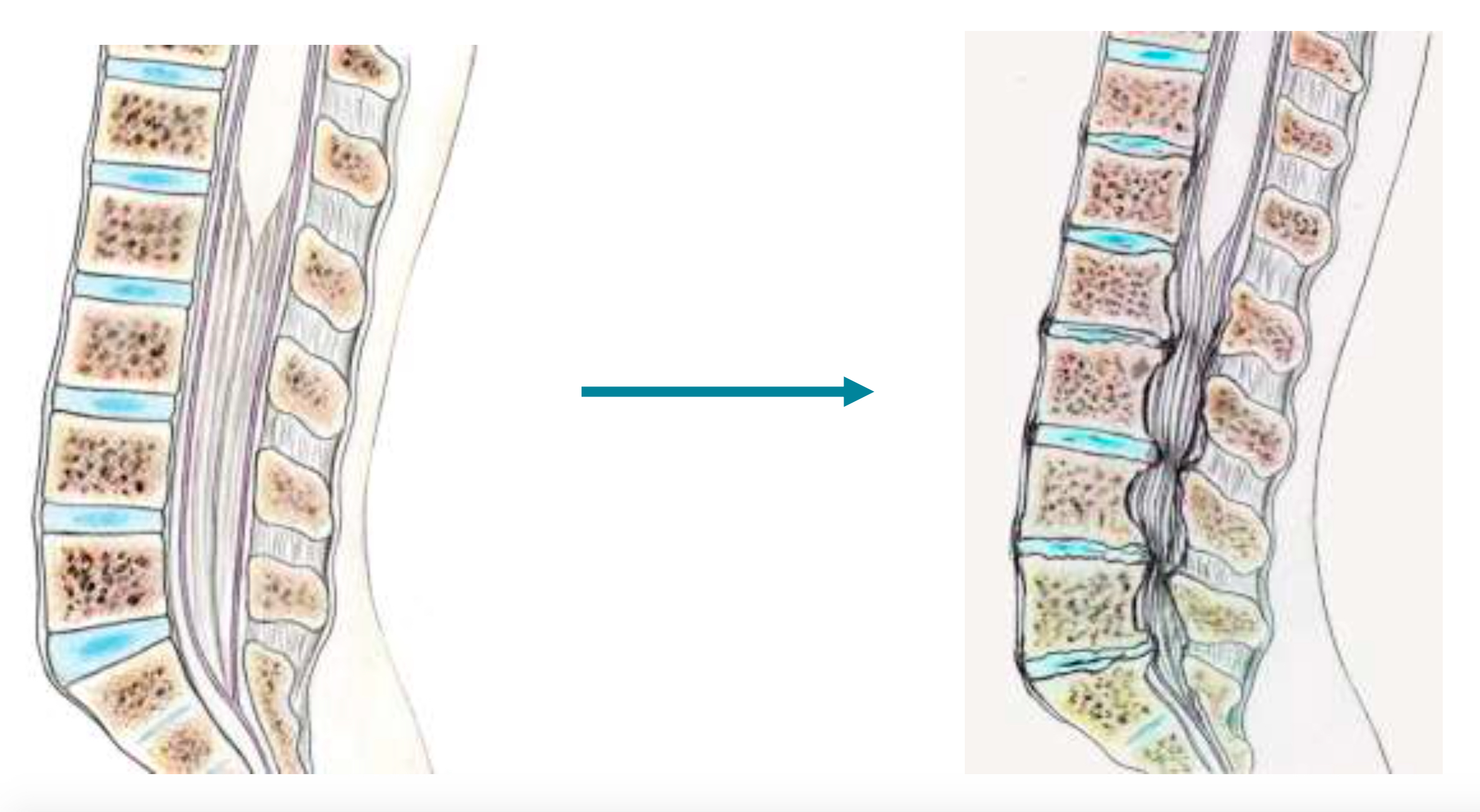
It’s a common pathology that most often develops gradually, secondary to vertebral osteoarthritis which narrows the vertebral canal through which the nerves for the lower limbs and sphincters pass.
The spinal column, also known as the rachis, is made up of 24 vertebrae stacked one on top of the other. They are connected by three joints: The intervertebral disc, which acts as a shock absorber between the vertebral bodies, and two posterior joints. Each vertebra has a hole in its center. Through this hole, also known as the spinal canal, pass the spinal cord and the nerves that control the sensations and movements of the whole body below the level of the head.
The size of the lumbar canal can be reduced by arthrosis linked to aging (wear and tear) of the joints. The same phenomenon occurs in the finger joints of the elderly. These tend to enlarge due to osteoarthritis, reducing the size of the spinal canal through which the nerves pass.
Other factors can narrow the canal, such as slipped vertebrae (spondylolisthesis), but this is rarer.
The nerves that transmit the movement commands sent by the brain to the various parts of the body circulate in this canal. The blood vessels supplying the nerves may also be compressed and no longer supply them with blood. Nerves can then become progressively damaged.
If a nerve is compressed, you may limp when walking, feel tired or have a tingling sensation in your legs after walking a certain distance.
These are pains, most often cramp-like, and a feeling of fatigue in the lower limbs when walking, sometimes with the impression that they will give out if walking continues. There is often associated lumbar pain. These cramps occur over increasingly shorter distances, forcing you to stop before you can resume walking(intermittent claudication). To limit these cramps, the patient spontaneously leans forward, thus artificially increasing the diameter of the vertebral canal. This is the “caddy” sign. While shopping, the patient spontaneously leans forward on his caddy, relieving pressure by opening the lumbar canal and foramen. Finally, if the narrowing of the canal becomes major, the patient may present neurological disorders (sensory, motor, urinary), but these generally appear gradually and insidiously. Patients with blocked arteries in the lower limbs (inferior limb arteritis) may present similar symptoms, but the patient’s examination, history and further tests will help to distinguish the difference. In this case, cramps are most often nocturnal.
- Static and dynamic lumbar X-rays: confirm vertebral osteoarthritis and show the stability or instability of the vertebrae in relation to each other.
- CT scan : confirms the diagnosis and the number of vertebral levels affected by the disease. CT scans are particularly good at visualizing bone.
- Myeloscanner or radiculography: If an MRI is not feasible (e.g. pacemaker), the surgeon may order a radiculography, which involves injecting contrast medium via a lumbar puncture and then performing an X-ray or CT scan. This test is rarely requested, as MRI has almost completely replaced it.
- MRI : thetest of choice. It provides all the information from the CT scan, but also shows the direct impact on the nerves, as well as the proportion of shrinkage related to bony structures and soft tissues (thickened ligaments, vertebral discs).
In the early stages of the disease, when symptoms are fairly discreet and the spinal canal is not very narrow, treatment can be medical. It combines analgesics, rehabilitation and, if necessary, the use of a lumbar belt. Local anti-inflammatory injections can also be used. In the more advanced stages, when disability becomes major and the vertebral canal extremely narrow, treatment is surgical.
Surgical treatment of narrow lumbar canal
The standard procedure(laminectomy) involves opening the vertebral canal by removing the elements that close off the spinal canal at the back: the spinous processes, the vertebral laminae and the yellow ligament that connect them.
Today, we use minimally invasive techniques, which involve making small incisions to re-calibrate the canal from the inside, without opening it completely and without removing the blades, spinous processes and all the ligaments. Only the compressive part is removed:
- Laminotomy
- Multi-stage windows
- Unilateral approach
- Trans-spinous approach
Our department specializes in these minimally invasive techniques.
Sometimes stability is compromised, for example in the case of spondylolisthesis (stair-step offset between 2 adjacent vertebrae). In such cases, the surgeon may propose arthrodesis (metal fixation).
