Trigeminal neuralgia is extreme facial pain characterized by intense, electric-shock-like attacks of facial pain that occur without warning and are most often triggered by touching specific areas of the face. Although the exact cause of trigeminal neuralgia is not fully understood, a blood vessel is often found to compress the trigeminal nerve. Medication, thermocoagulation, surgery and radiotherapy can be used to treat pain. Every treatment has its advantages and disadvantages.
What is trigeminal neuralgia?
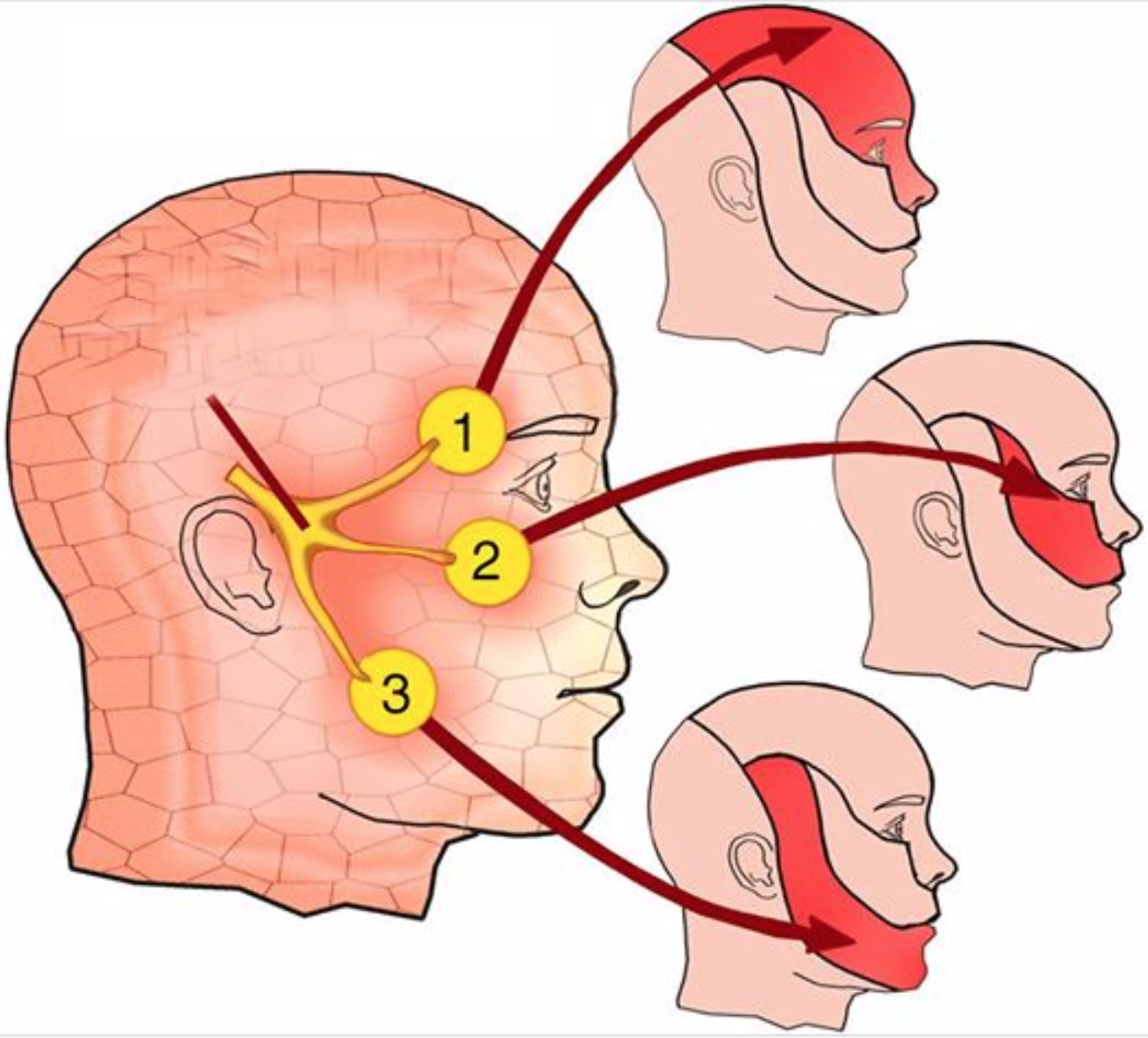
Neuralgia is intense pain caused by injury or damage to a nerve. The trigeminal nerve is the fifth (V) cranial nerve, with its orifices in the brain stem inside the skull. The trigeminal ganglion divides into three branches that exit the skull through bony orifices and are distributed to the face, where they transmit facial sensation and certain movements of the mandible:
- The ophthalmic division (V1) transmits sensitivity to the forehead and eyes.
- The maxillary division (V2) transmits sensitivity to the cheek, upper lip and palate.
- The mandibular division (V3) transmits sensitivity to the jaw and lower lip; it also enables movement of the muscles involved in mastication and swallowing.
When the trigeminal nerve is irritated, the result is an attack of intense pain. Also known as tic douloureux because of the uncontrollable facial contractions caused by the pain, trigeminal neuralgia is serious in its intensity and repercussions on many aspects of a person’s life. Trigeminal neuralgia is characterized by episodes of intense pain. This pain comes in repeated waves. The patient may initially present with short, mild attacks, with relatively long periods of remission. But trigeminal neuralgia can progress, causing longer and more frequent attacks of intense pain.
Patients describe an attack as a sensation of electric shock or crushing that may last a few seconds or minutes. Pain is often triggered by touching certain areas of the face, known as trigger zones, which, when touched, provoke an attack (Fig. 2). These areas are generally located near the nose, lips, eyes, ears or inside the mouth. As a result, some patients avoid talking, eating, kissing or drinking. Other activities, such as shaving or brushing your teeth, can also trigger pain. Wind on the face can sometimes trigger pain.
The pain may last several days or weeks, followed by remission for months or years.
The frequency of painful attacks increases over time and can become disabling.
A less common form of the disorder, called atypical trigeminal neuralgia, causes less intense, constant, dull burning or pain. This pain sometimes occurs with occasional stabs that can last a day or more. Atypical facial pain is more difficult to treat.
Many believe that the protective sheath of the trigeminal nerve is deteriorating, sending abnormal messages along the nerve. Like electricity in a telephone line, these anomalies disrupt the nerve’s normal signal and cause pain. Several factors can cause deterioration of this protective sheath: ageing, multiple sclerosis and tumours; but most often this deterioration is caused by an artery or vein compressing the nerve.
Some types of atypical facial pain may result from an infected tooth, temporomendibular joint involvement, sinus infections, shingles or post-herpetic neuralgia, or anterior nerve damage.
Trigeminal neuralgia affects 5 out of every 100,000 people, and slightly more women than men. Patients are generally middle-aged and older. Some people with multiple sclerosis may also develop trigeminal neuralgia.
What treatments are available?
Several treatments are available: drugs, surgery, thermocoagulation and radiotherapy. The first-line treatment is medication. When medication fails to control pain or causes significant side effects, a neurosurgeon can be consulted to discuss other solutions.
Medicines
Medications such as traditional analgesics (paracetamol, aspirin, morphine, etc.) or anti-inflammatories are not effective against trigeminal neuralgia. Anticonvulsants (Tegretol*, Lamictal*, Neurontin*, Lyrica*…) are prescribed to block pain signals from the nerve. These drugs are the initial treatment for trigeminal neuralgia, and are used as long as pain is controlled and side effects do not interfere with the patient’s activities. Around 80% of patients experience at least short-term pain relief with these drugs. For effective pain control, medication must be taken on a regular schedule (30 minutes before each meal) to maintain a constant blood level.
If the drug begins to lose its effectiveness, the doctor may increase the dose, switch to another drug or combine several drugs. Side effects may include drowsiness, instability, nausea, skin rashes and blood disorders. As a result, patients are monitored regularly and undergo blood tests to ensure that drug levels in the blood are not too high.
Surgery
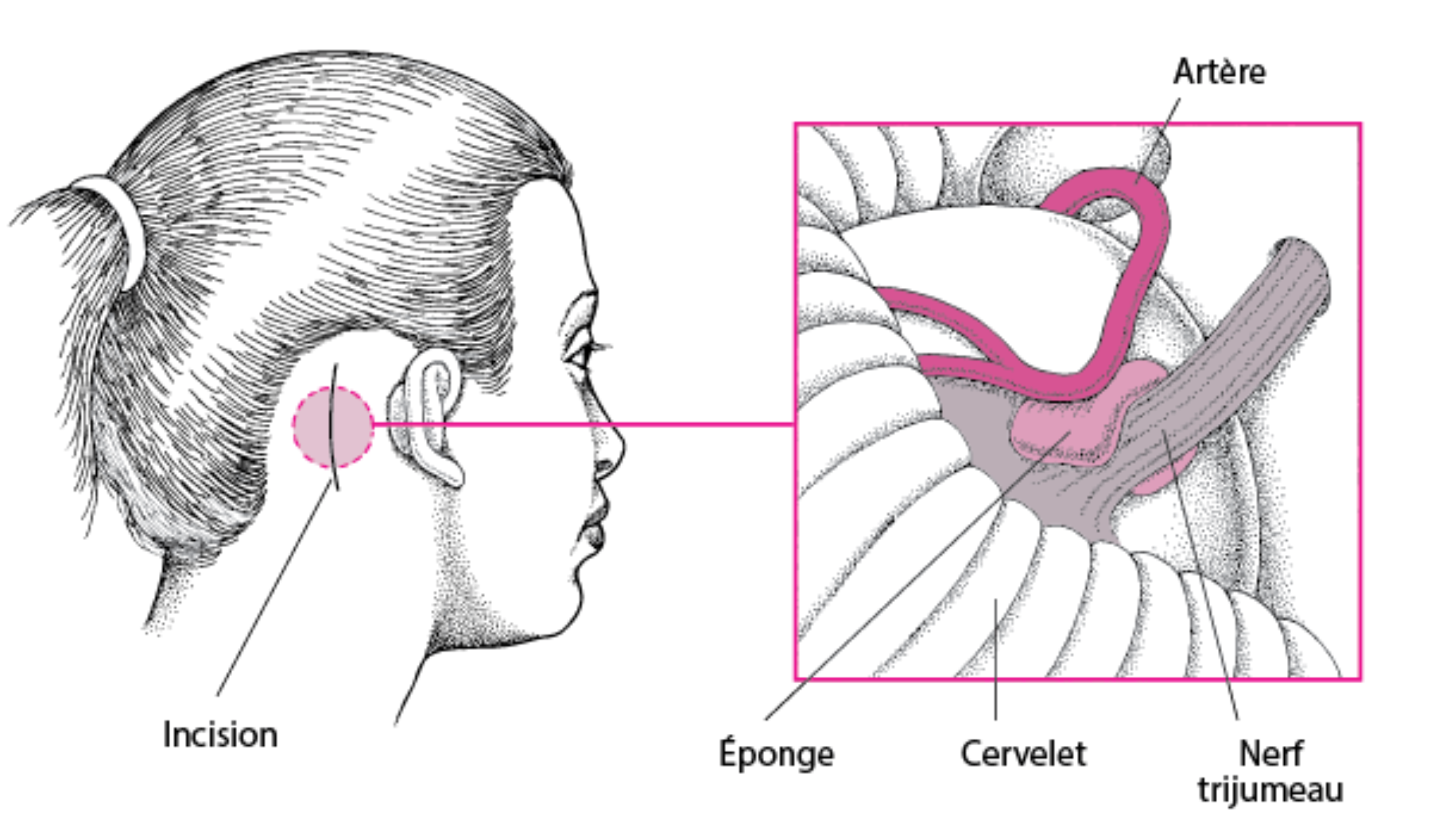
The purpose of the surgery is to prevent the blood vessel from compressing the trigeminal nerve.
Microvascular decompression (MVD) is a surgical procedure carried out under general anaesthetic which moves the vessel away from the nerve, interposing a small piece of Teflon between the nerve and the vessel to keep the vessel away from the nerve. Ideally, this piece of Teflon should not come into contact with the nerve.
This technique is also known as the Jannetta procedure, named after Prof. Peter Jannetta of Pittsburgh, USA, who developed and popularized it.
SEE PR JANNETTA’S PRESENTATION IN ENGLISH AT IRCAD STRASBOURG
Our department specializes in the treatment of essential neuralgia and offers a minimally invasive microvascular decompression technique.
The procedure involves a small arched incision 2-3 cm behind the ear. A hole the size of a 1 euro coin is then made in the skull bone. The dura mater enveloping the brain and cerebellum is then opened and the nerve examined under a microscope. The vessel that compresses it is then pulled away, and a small piece of Teflon keeps it there.
This procedure provides immediate pain relief in 90% of patients. Around 20% of patients experience a recurrence of pain within 10 years. The main advantage of this procedure is that it causes little or no facial numbness. The major drawbacks are the risk of anesthesia and the risk of undergoing surgery close to the brain.
Radiosurgery
Radiosurgery is a radiotherapy technique that uses highly focused beams of radiation to destroy some of the pain-producing fibers of the trigeminal nerve roots. The two main technologies are the Gamma Knife and linear gas pedal systems such as the BrainLab Novalis. A frame or face mask is attached to the patient’s head to pinpoint the exact location of the nerve on an MRI scan, and to keep the head perfectly still during treatment. Highly focused radiation beams are delivered to the trigeminal nerve root (Fig. 6). In the weeks following treatment, a lesion (wound) develops where the radiation occurred.
Pain relief may not occur immediately, but rather gradually over time. As a result, patients continue to take painkillers for some time. The success of radiosurgery becomes evident when analgesics are reduced or eliminated. After 4 weeks, around 50% of patients will experience pain relief with no or reduced medication. After 8 weeks, 75% will have pain relief with no or reduced medication. Complications include facial numbness and dry eyes. In around 30% of patients, pain recurs 3 to 5 years after treatment. Radiosurgery can be repeated; however, the risk of facial numbness is increased.
Outpatient needle procedures
Needle procedures are invasive needle techniques for reaching the trigeminal nerve through the face without skin incision or skull opening. They are performed with a hollow needle inserted through the skin (percutaneously) of the cheek and placed in the trigeminal nerve, passing through the base of the skull. The aim of rhizotomy procedures is to damage an area of the trigeminal nerve to prevent it from sending pain signals to the brain. Damage to the nerve causes facial numbness in this area. This facial numbness is an expected result and is necessary to achieve long-term pain relief. These outpatient procedures are generally performed under local anaesthetic and light sedation. Patients usually go home the same day.
Radiofrequency rhizotomy, also known as thermocoagulation, uses a heating current to selectively destroy some of the trigeminal nerve fibers that produce pain. While the patient is asleep, a hollow needle and electrode are inserted through the cheek into the nerve. The patient is awakened and a weak current is passed through the electrode to stimulate the nerve and cause tingling in the territory where the painful attacks are located, thus verifying that the needle is in the part of the nerve that is causing the pain. Once the painful area has been localized, the patient is put back to sleep and a heating current is passed through the electrode to damage this part of the nerve.
Thermocoagulation brings immediate pain relief to 95% of patients. Around 20% of patients experience a recurrence of pain within 10 years.
Complications can include double vision, jaw weakness, loss of corneal reflex, dysesthesia (uncomfortable numbness) and, very rarely, anesthesia dolorosa. Partial facial numbness in the area where pain existed is expected. Other complications, such as blurred vision or chewing problems, are usually temporary.
Future patient?
Your stay is our priority, and we set up a patient pathway program for your operation, admission
and intervention, right up to your discharge. Please do not hesitate to contact us if you have any questions.
