CHORDOMAS are rare tumors that develop in the bones at the base of the skull or the spinal column. This is a complex lesion requiring specialized management by a multidisciplinary team accustomed to dealing with this type of injury. Our team has some of the world’s most extensive experience in the treatment of chordoma.
Chordoma, a rare bone cancer – Le Magazine de la santé – Video Youtube
Chordomas develop from residues of the notochord. The notochord is an embryonic structure that forms the axis of development of the fetus and participates in the development of the spinal column.
The notochord disappears when the fetus is around 8 weeks old, but some notochord cells do not disappear and persist in the bones of the spine and skull base. The reason why some of these cells develop into chordomas is not yet known, but research is progressing.
The vast majority of chordomas occur randomly and are not hereditary. As with all tumors, there are certain genetic changes in chordoma cells. For example, over 95% of individuals with a chordoma have an abnormality in the DNA sequence of a gene called brachyuria. This anomaly increases the risk of developing a chordoma, but does not in itself cause a chordoma.
There are around 80 new cases in France every year. At any given time, less than one person in 100,000 is living with a chordoma (prevalence).
Chordoma is most often diagnosed in people aged 50-60, but can occur at any age.
There is also a slight male predominance, with a ratio of around 2 men to 1 woman.
Familial chordomas are very rare, and only a handful of cases have been identified.
Around 40% of chordomas form in the skull base and craniocervical hinge, 30% in the bones of the mobile spine and around 40% in the sacrum.
Chordomas of the skull base are generally located in a bone called the clivus. These are deep-seated lesions, generally located in the center of the skull, close to critical structures, which are difficult to access and complex to treat. Skull base chordomas are sometimes called brain tumors because they can grow inwards from the skull towards the brain, but they don’t actually develop from brain cells.
They can also occur in the cervical spine and lumbar spine (lower back). These zones make up the “mobile” column. Locations in the thoracic spine are rarer.
In 40% of cases, they also occur in the sacrum. They are located more or less high on the sacrum and are more or less complex to remove, depending on the relationship with the nerves to the sphincters and the rectum in front.
What are the symptoms?
Chordomas usually develop slowly, and symptoms are usually delayed.
Symptoms vary depending on the location of the chordoma.
At the base of the skull, the most frequent symptoms are headaches and double vision. Other symptoms may include visual loss, hearing loss, difficulty swallowing, hoarseness, walking difficulties, motor weakness…
Spinal chordomas usually manifest as pain, tingling or weakness in a limb.
Chordomas of the sacrum are often discovered at a late stage, and manifest as pain, urinary problems and even urinary and faecal incontinence.
How is the diagnosis made?
The tests used to identify tumors are CT scans and, above all, MRIs. The very specific appearance of chordomas on MRI often leads to a strong suspicion of this diagnosis.
Specific MRI sequences are required to pinpoint the diagnosis. As this is a rare tumor, radiological diagnosis requires experienced radiologists.
Are there different types of chordoma?
Once removed and analyzed, different types of chordomas can be distinguished:
- Typical chordoma
- Chondroid chordoma
- More aggressive dedifferentiated chordoma. This type of chondroma is rare, and more common in young children.
The latest WHO classification of 2020 now defines 3 categories:
- Conventional chordoma, including typical and chondroid chordomas. This category accounts for the majority of chordomas.
- Dedifferentiated chordoma, very rare. This type of chondroma most often occurs during the evolution of a known chondroma, and particularly in cases of recurrence after irradiation.
- Poorly differentiated chordoma. This is a new entity defined by the presence of the loss of a protein, INI1 (linked to the deletion of a SMARCB1 gene). This type of chordoma is more aggressive than conventional chordoma, but can also respond to targeted medical treatment.
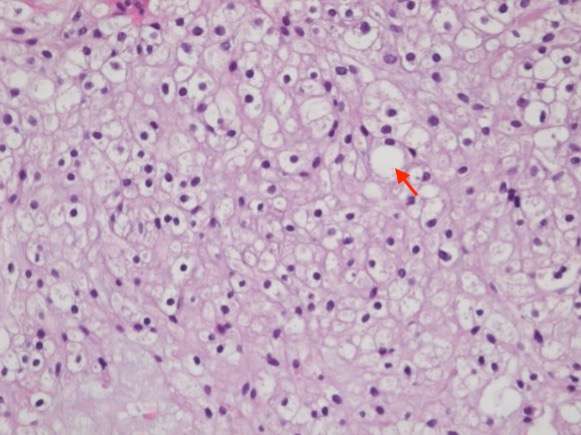
Microscopic view of a conventional chordoma fragment, after staining with Hemalun-Eosin-Safran (HES). Magnification x 400. Vacuolated cells (red arrow) correspond to physaliphore cells typical of chordomas.
What is the treatment?
-
Multidisciplinary approach
A multidisciplinary approach is vital in the management of these lesions.
We collaborate with several teams in the management of these tumors:
- Neuroradiology Department, Lariboisière Hospital
- the Orsay proton therapy department,
- Institut Curie: Dr Hamid Mammar, Dr Valentin Calugaru
- the radiotherapy department of the Pitié Salpetrière Hospital: Dr Loic Feuvret
- Gustave Roussy Institute: Dr Stéphanie Bolle
- Necker Hospital and Pediatric Neurosurgery Department: Dr Kevin Beccaria
A national multidisciplinary “chordoma and chondrosarcoma” meeting, organized by the Neurosurgery Department, brings together all those involved in the care of chordoma patients, and takes place once a month. During this meeting, all the French teams have the opportunity to present their patients’ files, in order to discuss the different treatment options and choose the most suitable one.
-
Is a biopsy necessary?
In the skull base and cervical spine, a biopsy is rarely necessary.
In the lumbar spine and sacrum, a biopsy may be taken to confirm the diagnosis. However, it is not necessary in all cases, as the radiological diagnosis is often conclusive. It must be carried out by trained teams under special conditions to avoid tumor dissemination along the biopsy route.
-
Surgical treatment
Surgery should be performed in centers with experience in skull base neurosurgery and/or spinal chordoma surgery.
In the case of the skull base, these are complex lesions requiring mastery of a number of specific skull base surgical techniques. Incomplete treatment in a center with insufficient experience in this type of surgery can complicate a repeat operation and compromise the chances of complete excision. Our team has internationally recognized experience in the management of chordomas, with one of the highest numbers of patients treated in the world.
The aim of surgery is to remove the entire tumor while preserving the nerve structures in the immediate vicinity. This is not always possible, particularly at the base of the skull, due to the presence of critical structures in the immediate vicinity of the tumor or which cross the tumor. In this case, the aim is to reduce the size of the lesion as much as possible, and move it away from the normal structures at risk, which are compressed by the tumor, in preparation for radiotherapy. This high-risk surgery requires a medical team (neurosurgeon, radiologist, ophthalmologist, anesthetists, resuscitators) and paramedical staff specialized in the care of these patients.
In the sacrum, “en bloc” resection of the tumor, passing beyond the tumor’s limits without ever crossing the tumor’s external capsule, is the optimal technique. This is the technique that gives the best chance of recovery. However, this is not always possible for lesions high on the sacrum, except at the cost of sacrificing sphincter genital functions. Our strategy is to give maximum priority to function, using microsurgical techniques that preserve a maximum number of nerve roots and thus the associated sphincter function, while most often performing en bloc excision. When nerve sacrifice cannot be avoided, the strategy is defined with the patient, according to his or her priorities.
Radiotherapy
Chordomas are tumors with a strong tendency to local recurrence. Surgical treatment must therefore be complemented by high-dose radiotherapy. The technique most often used is proton therapy. It is carried out at the Orsay proton therapy center by specialized radiotherapists:
– Dr Hamid Mammar
– Dr Valentin Calugaru
– Dr Loic Feuvret
– Dr Stéphanie Bolle
Radiosurgery is sometimes proposed for small lesions at a distance from high-risk structures, or in the event of minor localized recurrence.
-
Chemotherapy
In the event of tumor recurrence, re-intervention is usually possible and proposed.
After surgery, in the event of a new recurrence or when surgery is not possible, chemotherapy may be proposed. Therapeutic trials are underway to evaluate the efficacy of new treatments, and may be proposed.
Each patient’s prognosis is unique and depends on many factors: age, type of chordoma, volume at diagnosis, location, type of treatment available, whether or not the tumour has been completely removed….
Evolution
Their evolution is often favorable, but requires aggressive treatment: surgery and proton therapy.
One of their characteristics is their tendency to grow back locally, i.e. where they were initially located. This is known as local recurrence. In around 30% of patients, the tumour spreads to other parts of the body as it progresses. If chordomas spread to other parts of the body (metastases), the most common places to which they spread are the lungs, liver, subcutaneous tissue or lymph nodes. Metastases, when they occur, generally appear late in the course of the disease, when the primary tumor recurs. They are rarely discovered at the time of initial diagnosis, and are often quite well tolerated.



