Intracranial epidermoid cysts are rare, benign lesions that are almost always congenital, i.e. present from birth. They result from the aberrant inclusion of ectodermal (skin-forming) elements during neural tube closure, between the 3rd and 5th week of embryonic development. More simply put, it’s a bit of cutaneous tissue (skin) that is captured inside the cranial cavity when the embryo is formed and then behaves like skin, i.e. producing squames (a thin flake of dead skin that detaches from the epidermis), but in the wrong place.
They account for 0.3% to 1.8% of all intracranial neoplasms.
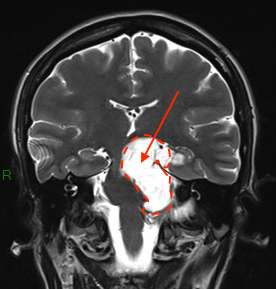
They are located in the sub-arachnoid spaces around the brain, brain stem and cerebellum.
They are most often located deep beneath the brain or in front of the brainstem and cerebellum, making them difficult to remove. They are considered to be injuries to the base of the skull.
The most common locations are :
- the cerebellopontine angle
- suprasellar regions
- the sylvan valley
- the ventricular system, in particular the 4th ventricle,
- pineal region.
Epidermoid cysts are also known as “pearly” tumors, due to their pearly-white color and nippled appearance.
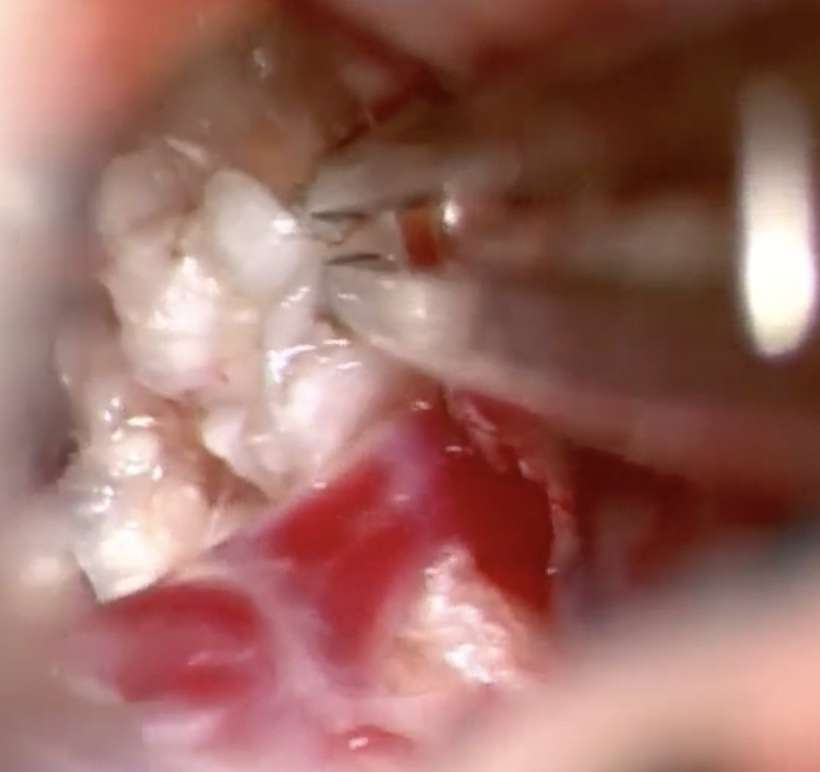
Histologically, they consist of a stratified, keratinized epithelial wall delimiting a cavity in which the degradation products of desquamated epithelial cells accumulate in the form of an amorphous material rich in keratin and cholesterol.
The rarer dermoid cyst does not usually have the milky-white appearance so characteristic of its epidermoid counterpart. It is more variable, more heterogeneous, due to the diversity of materials that collect in its cavity. The epithelial lining is identical, but its wall also contains dermal elements: hair follicles, sebaceous and sweat glands, and sometimes even fat lobules. The cystic content is thus a more or less heterogeneous amalgam of keratin, cholesterol, sebaceous and sweat secretions, giving a more yellowish appearance, often with hairs.
They grow very slowly and symptoms appear late.
Symptoms vary according to tumour location:
– headaches, but it’s often difficult to tell whether they’re related to the lesion or not,
– dizziness,
– balance disorders,
– damage to one or more cranial nerves: facial pain, double vision, hearing loss, facial paralysis, facial hemispasm, reduced vision, visual field amputation due to direct tumor compression of the nerves.
– epileptic seizures
How is the diagnosis made?
On a CT scan, an epidermoid cyst typically appears as an iso or hypodense, heterogeneous mass with irregular contours and no contrast or perilesional edema.
Diagnosis is confirmed byMRI, in particular by their hypersignal on diffusion sequences. Diffusion sequences are essential for confirming the diagnosis on MRI.
Treatment
Progressing very slowly, they are usually monitored by regular MRI scans.
Surgical treatment is proposed in the event of symptoms. If symptoms are moderate and the risk of surgery is considered significant, surveillance may be preferred in the first instance.
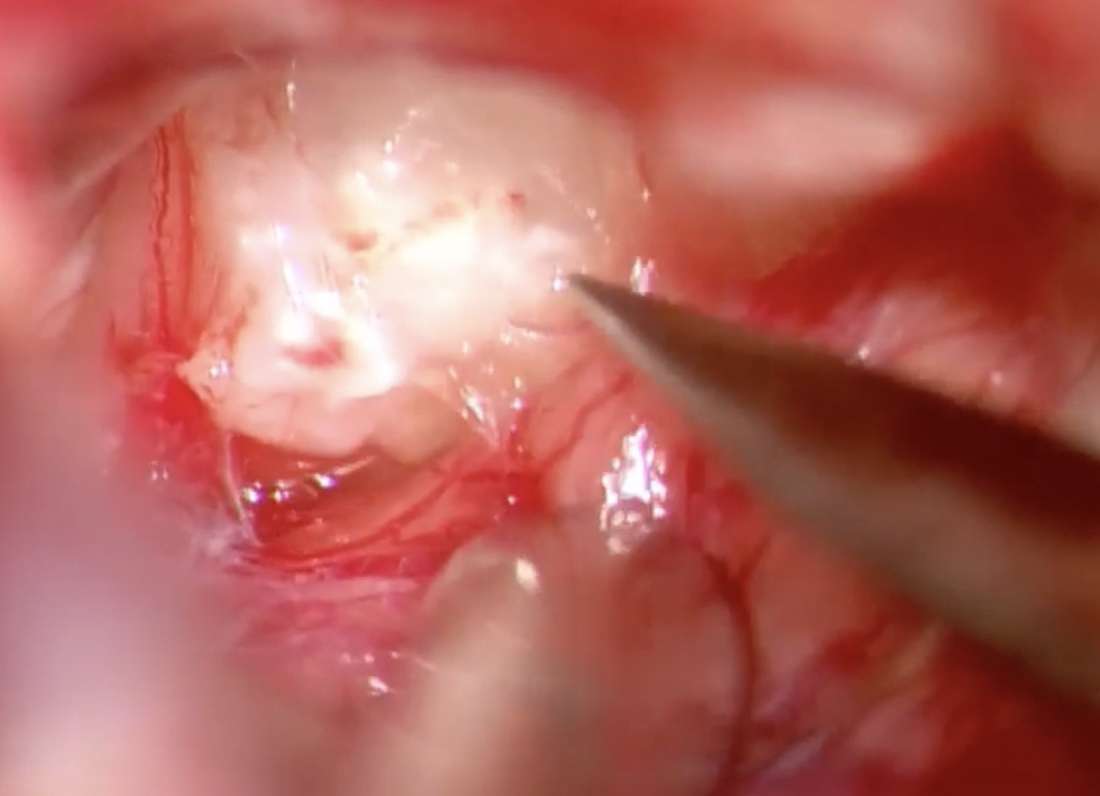
The treatment of choice for epidermoid cysts is total resection of the tumor, including the cyst capsule that produces the cyst contents. In some cases, however, total resection is impossible, due to the location of the cyst and its close relationship with neuronal or vascular structures. In this case, part of the capsule is left in place, with a high risk of recurrence. But it is even more difficult, if not impossible, to remove the capsule, and thus heal, in a second operation, because the scar left by the first operation makes it even more difficult to separate the capsule from the surrounding nerves and vessels. That’s why it’s important to try to remove the capsule as much as possible during the first operation.
The surgical approach to the cyst depends on its location. Some large cysts require complex approaches to the skull base to enable complete removal while preserving nerve and vascular structures.
Course and prognosis
They develop very slowly. After surgery, if part of the capsule is left in place, the risk of the cyst reappearing is high, but often after many years. A reoperation is sometimes necessary.
Overall, the prognosis is good, but epidermoid cysts often require complex, high-risk surgery, requiring surgical expertise in this type of lesion.
Malignant transformation of an epidermoid cyst is exceptional.
