When the spinal canal is narrowed in the cervical region (neck), the spinal cord and the nerves emerging from it can become compressed.
Causes
The most common cause is osteoarthritis. Osteoarthritis is a well-known phenomenon that deforms joints over time, as can be seen in elderly people’s hand joints, for example. The same phenomenon in the joints of the cervical spine can lead to compression of the spinal cord and nerves passing between these joints. Other causes are possible: a constitutional cause, i.e. linked to the development of the spinal column, or a tumoral cause in the case of tumors located in the cervical vertebrae.
This pathology causes compression of the spinal cord and the nerves that exit the spinal column between the vertebrae (spinal nerves), in the direction of the arms. This can lead to pain in the arms, tingling sensations, weakness in the arms and hands, problems with balance and walking due to compression of the spinal cord, or problems with urinary and faecal continence.
The radiological workup consists of a CT scan and MRI of the cervical spine.
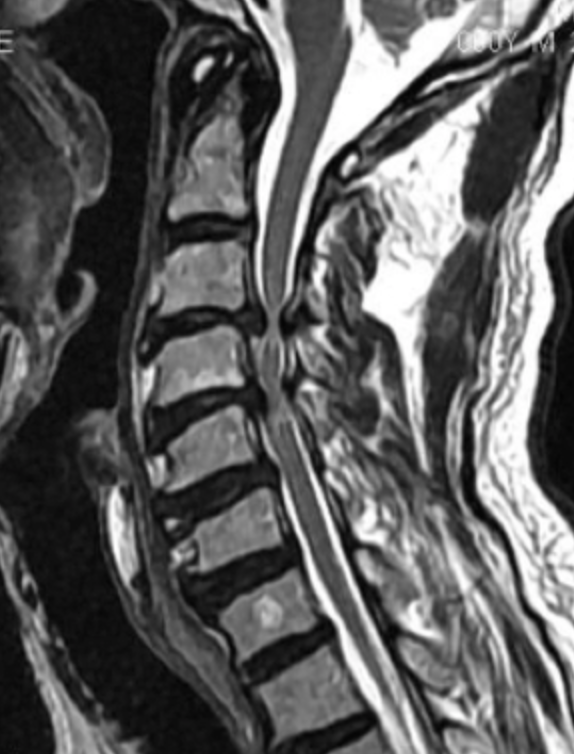
C3-C4 and C4-C5 cervico-arthrosic myelopathy leading to spinal cord compression and suffering.

The surgeon will sometimes ask for a dynamic MRI in flexion and extension to see if compression is accentuated in certain positions.
An electromyogram can also be performed to assess nerve conduction in the nerves of the upper limbs.
More information on EMG electromyography
In cases of suspected spinal cord compression, somaesthetic and motor evoked potentials are also performed to measure the speed of conduction of information in the spinal cord from the brain to the limbs (motor evoked potentials) and from the limbs to the brain (somaesthetic evoked potentials).
More information on evoked potentials
X-rays of the shoulder are sometimes performed, as osteoarthritis of the shoulder can give rise to similar symptoms in the arms.
Following radiological and electrophysiological assessment, surgical treatment may be proposed to decompress the cervical spinal cord and/or nerves. Surgery is sometimes urgently required in cases of rapid neurological deterioration, as neurological recovery in cases of severe spinal cord injury is uncertain. The main purpose of surgery is to prevent further worsening, but it cannot lead to systematic recovery. The procedure is performed under general anaesthetic, and most often requires a urinary catheter to be inserted once the patient is asleep, which is usually removed the day after the operation. There are several possible surgical modalities, depending on the type of involvement on CT and MRI scans.
- Objective: the aim is to decompress the spinal cord and nerves while ensuring spinal stability.
- Surgical approach Depending on the type, location and extent of spinal cord compression, an anterior approach, on the front of the neck, or a posterior approach, on the back of the neck, may be proposed. To increase the safety of the procedure, this neurological release can be performed under neurophysiological control of the spinal cord. Electrodes are placed on the skull and limbs, and a computer continuously monitors the passage of weak electrical impulses through the spinal cord.
- Vertebral fusion or “arthrodesis”: Vertebral fusion is most often proposed in cases of anterior decompression. This involves fusing the two vertebrae together, after removing the intervertebral disc. Removal of the intervertebral disc is then necessary to decompress the spinal cord and nerves. The impact on mobility is usually very slight, as the spine is often already very stiff due to osteoarthritis, reducing neck flexibility.
- Disc prosthesis: In certain special cases, a disc prosthesis can be used instead of fused vertebrae to maintain some mobility.
A drain is sometimes inserted at the end of the procedure to prevent the formation of a postoperative cervical hematoma.
What happens after the operation?
After the operation, the patient is taken to the recovery room to be monitored before returning to the room, usually two to four hours later.
You can get up for the first time on the day of the operation or the following morning. The physiotherapist is on hand in the days following the operation to help the patient resume activity and give advice on what to do next.
Pain is generally very moderate, but painkillers are given both as a preventive measure and in case of pain.
Post-operatively, the drain, when present, is retained for 24 to 48 hours.
This surgical procedure requires hospitalization for a few days and temporary immobilization with a foam cervical collar.
Very often, the skin is closed using an intradermal overjet, which is absorbable (the threads are under the skin). There are no wires to remove.
Driving must be suspended during the convalescence period until the follow-up consultation, which generally takes place 4 to 6 weeks after the operation.
